Status: North Dakota does not have any active cases of measles, at this time. The last case of measles in North Dakota was in 2011. In the event of a confirmed measles case in ND, this page will be updated as soon as possible.
Updated: March 24, 2025
About Measles
Measles (Rubeola)
Measles is a highly contagious viral disease with an abrupt onset. Measles commonly causes fever, rash, cough, and runny nose. Measles may cause serious complications and result in pneumonia, swelling of the brain, convulsions, deafness, long-term intellectual disabilities, and death in 1-2 out of 1000 infections. Measles is also known as rubeola, which should not be confused with rubella, another vaccine-preventable viral rash illness that is uncommon in developed countries, or roseola, a common, mild rash illness that occurs in children.
Transmission
Measles is spread person-to-person when an infected person coughs or sneezes. This virus is extremely contagious because particles are very small and stay in the air for up to two hours after a contagious person has been in an area. Because it is airborne, it can spread between rooms of a building via the air duct system. When a person with no immunity through immunization or prior infection is exposed to measles virus, the probability of contracting disease is very high – over 90% for a single encounter. A single person with measles spreads disease to an average of 18 other people if those people are not immune due to immunization or prior infection.
Symptoms
Symptoms typically appear within 7-12 days of exposure but may appear up to 21 days after exposure. Symptoms almost always first include a fever, followed by a characteristic flat, blotchy rash that starts on the face and neck and progresses down the body. Most people with measles will also develop flu-like symptoms, including a cough, runny nose, and pink or watery eyes. People with measles may also develop tiny white spots inside their mouth called “Koplik spots.”
Diagnosis
Suspected measles cases should be reported to the ND HHS immediately. Measles diagnosis requires an oral PCR swab test and may also include a blood sample for IgM. Tests can be routed to ND HHS Laboratory Services for testing. For questions and recommendations about testing, please contact the ND HHS Immunization Unit. Providers should consider recent travel and vaccination status, when assessing the likelihood of measles and need to test.
Special Considerations for Measles Work-Up in Patients
Measles is extremely contagious and dangerous to infants under one year old, who have not had an opportunity to be vaccinated, or patients who are immunocompromised. If a patient or family suspects measles, they should call ahead before presenting to a clinic or hospital. Health care providers may wish to meet a patient outside and perform drive-up assessment and testing. Suspect measles patients should not enter or occupy the waiting area of a health care facility if this can be avoided. If measles is suspected, the patient and all exposed to them should be given a mask immediately and isolated in a room with negative pressure if possible. Rooms with suspect measles cases should be sanitized and closed to patients for a minimum of two hours following the suspect measles case.
Treatment
There is no specific antiviral treatment for measles. Antibiotics may be used in cases that have developed secondary bacterial infections. Supportive care can be offered to measles patients, and resources often demand that families care for measles patients at their home. In some cases, measles cases will require hospitalization. In recent outbreaks, up to 20-40% of measles patients have been hospitalized.
Prevention
• Measles is easily prevented through vaccination. Measles vaccine is extremely safe, and after the two recommended doses are given, over 98% effective.
• The combination measles-mumps-rubella vaccine (MMR) and a vaccine that includes these components plus one to prevent chickenpox (MMRV) are the measles-containing vaccines given in the United States since the 1960s.
• People living outside the U.S. may have been given a measles-only vaccine, which is also effective, but may be repeated to prevent mumps and rubella. MMR vaccine is required for school entry, in North Dakota.
• Over 100 peer-reviewed scientific articles and hundreds of independent researchers have studied and confirmed the safety of the measles vaccine in all ages, races, and backgrounds.
• People born prior to 1957 are assumed to have immunity to measles, since the disease was so widespread prior to routine vaccination. People working in health care may need to receive MMR vaccine regardless of date of birth.
• Children under one year old are not routinely given MMR vaccine, yet, and so immunity of those around them to measles is especially important. If an infant is traveling to an area with measles before 12 months of age, but after six months of age, they may receive one dose of MMR vaccine for protection against measles but will need to repeat this dose after they are one year old.
• A second measles vaccine is given at four to six years old but may be given as early as 28 days after the first dose is administered.
• People exposed to measles who are unable to receive MMR vaccine may be offered measles vaccine or measles immune globulin (IG) as a form of post-exposure prevention, but this is much less effective than vaccination prior to exposure.
Cost should not be a barrier to vaccination. The Vaccines for Children (VFC) Program provides all recommended vaccines to children who are American Indian, uninsured or underinsured, and Medicaid-eligible. Many recommended vaccines are also available for uninsured adults. Vaccines are available at your local health care provider, public health department or pharmacy.
Exclusion Guidance
Measles cases are infectious from four days prior to the onset of the rash until four days after the rash developed and should be excluded from childcare, school, and all activities until this period has passed. Patients with active measles should isolate at home away from unimmune family members. Unimmunized (zero doses of MMR) or under-immunized (one dose of MMR) may receive a dose of MMR within 72 hours of exposure to possibly interrupt development of disease. Unimmunized people who are exposed to measles must quarantine at home and be excluded from school or childcare for 21 days after exposure, regardless of the reason for not being immunized.
Resources:
1. Centers for Disease Control and Prevention. (2020, November 5). CDC Measles. Centers for Disease Control and Prevention. Retrieved January 30, 2024 from https://www.cdc.gov/measles/index.html.
2. Kimberlin, D. W., Barnett, E. D., Lynfield, R., Sawyer, M. H. (2021) Red Book: 2021-2024 Report of the Committee on Infectious Diseases. 32nd ed. American Academy of Pediatrics. [Management and Prevention of Infectious Diseases; Measles] [pages 503-519]. Revised January 30, 2024
About Measles Vaccine
Am I up-to-date for measles immunization?
You are considered immunized against measles if you have written documentation (records) showing at least one of the following:
- You received two doses of measles-containing vaccine, and you are a(n) —
- school-aged child (grades K-12)
- adult who will be in a setting that poses a high risk for measles transmission, including students at post-high school education institutions, health care personnel, and international travelers.
- You received one dose of measles-containing vaccine, and you are a(n) —
- preschool-aged child (12 months to 4 years)
- adult (born in 1957 or later) who will not be in a high-risk setting for measles transmission.
- Laboratory confirmed that you had measles at some point in your life.
- Laboratory confirmed that you are immune to measles.
- You were born before 1957.
For international travelers
The best protection against measles is if you have written documentation (records) showing at least one of the following:
- You received one dose of measles-containing vaccine, and you are an infant aged 6–11 months
- You received two doses of measles-containing vaccine, and you are a person 12 months or older
- Laboratory confirmed that you had measles at some point in your life
- Laboratory confirmed that you are immune to measles
- You were born before 1957
Do I need an additional booster shot for measles as an adult?
No. CDC considers people who were vaccinated as children according to the U.S. vaccination schedule protected for life, and they do not ever need a booster dose. Adults born before 1957 are protected due to previous infection. If you’re not sure whether you are fully vaccinated, talk with your healthcare provider or local public health unit. North Dakota residents may also have immunization history in the North Dakota Immunization Information System and may find that by visiting our website at https://hhs.nd.gov/IRR.
Do people who received the killed measles vaccine in the 1960s need to be revaccinated with the current, live measles vaccine?
Not many people fall into this group; the killed vaccine was given to less than one million people between 1963 and 1968. Also, most people don’t know if they got the killed vaccine during this time. If you’re unsure whether you fall into this group, you could ask your healthcare provider to test your blood to determine whether you’re immune or you can just get a dose of MMR vaccine.
How do I find my immunization record?
The North Dakota Immunization Information System (NDIIS) includes immunization records for children and adults who were vaccinated in North Dakota. The NDIIS was started in the mid 1990’s, so immunizations administered prior to that may not be available. You can request a copy of your NDIIS record at your healthcare provider’s office, your local public health unit, or from the North Dakota Department of Health and Human Services (ND HHS) at Immunization Record Request | Health and Human Services North Dakota. If your record is not in the NDIIS, you will have to contact your healthcare provider and/or parent to obtain your record. Some adults may be unable to find their immunization records.
Is it safe to have another measles vaccine if you had one as a child but can’t find a record of it?
Yes, no safety concerns have been identified due to receiving an additional dose of MMR.
How well does the MMR vaccine work?
MMR vaccine is very effective at protecting people against measles, mumps, and rubella. One dose of MMR vaccine is 93% effective against measles. Two doses of MMR vaccine are about 97% effective against measles
Who should not get the MMR vaccine?
Some people should not get the MMR vaccine. Tell your health care provider if you:
- Are pregnant or think you might be pregnant. Women should avoid getting pregnant for at least one month after getting MMR vaccine.
- Have any severe, life-threatening allergies. A person who has ever had a life-threating allergic reaction after a dose of MMR vaccine or has a severe allergy to any part of the vaccine, may be advised not to be vaccinated.
- Have a weakened immune system due to disease (such as cancer or HIV/AIDS) or medical treatments (such as radiation, immunotherapy, steroids, or chemotherapy).
- Have a parent, brother, or sister with a history of immune system problems.
- Have ever had a condition that makes them bruise or bleed easily.
- Have recently had a blood transfusion or received other blood products. You may be advised to postpone MMR vaccination for three months or more.
- Have tuberculosis.
- Have gotten any other vaccines in the past four weeks. Live vaccines given too close together might not work as well.
- Are not feeling well. Mild illness, such as a cold, is usually not a reason to postpone vaccination. Someone who is moderately or severely ill should probably wait. Your health care provider can advise you.
Cost should not be a barrier to vaccination. The Vaccines for Children (VFC) Program provides all recommended vaccines to children who are American Indian, uninsured or underinsured, and Medicaid-eligible. Many recommended vaccines are also available for uninsured adults. Vaccines are available at your local health care provider, public health department or pharmacy.
Resources:
Centers for Disease Control and Prevention. (2024, May 29). CDC Measles (Rubeola). Centers for Disease Control and Prevention. Retrieved March 6, 2025 from https://www.cdc.gov/measles/index.html
Should I receive a dose of measles vaccine?
People who have received immunizations in North Dakota can check their NDIIS immunization history (and that of their minor children) online through Docket® or request immunization certificates by mail. Please note that people born before electronic health records may not have childhood immunizations recorded, in this system.
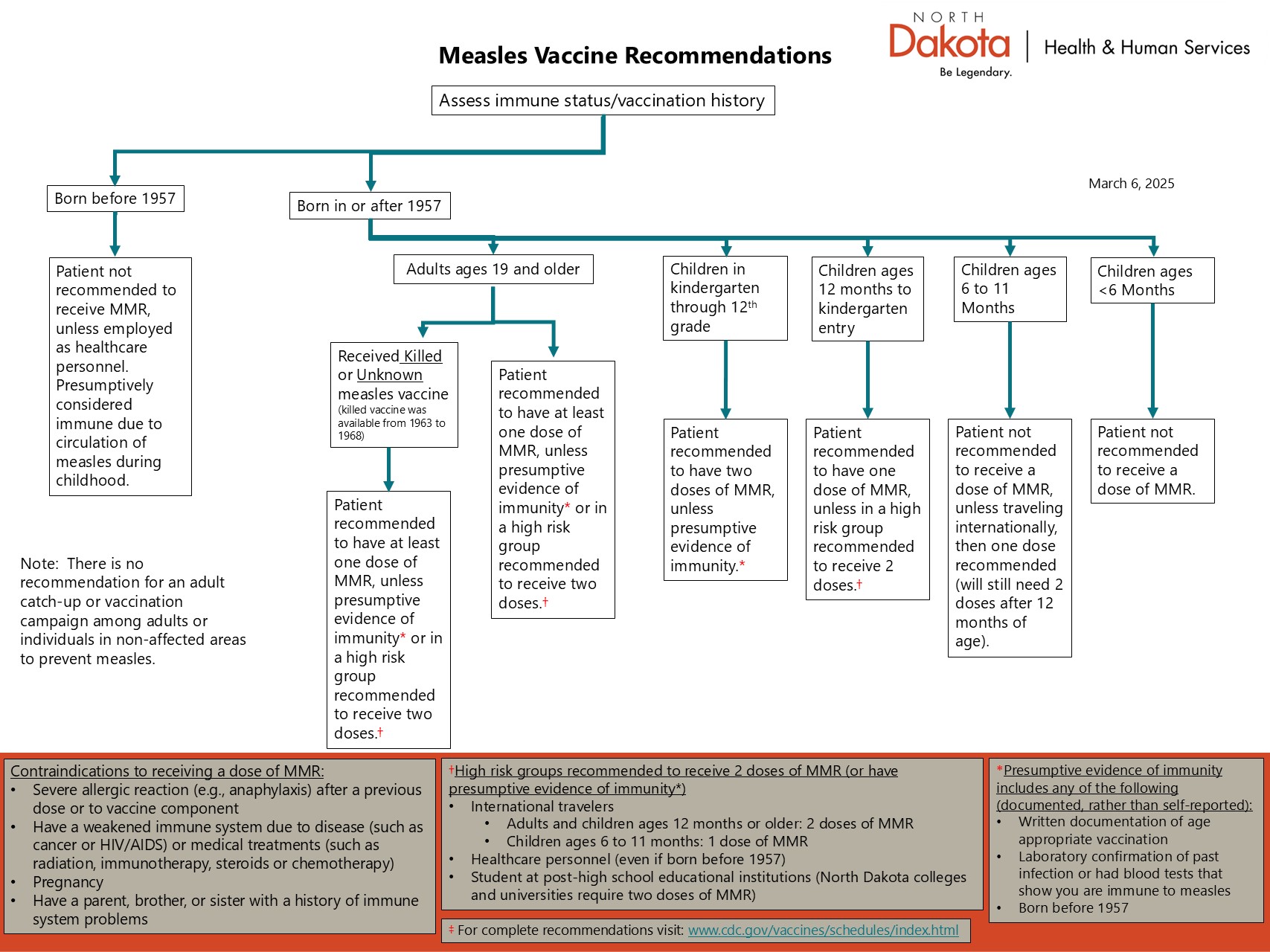
Please use this chart to determine whether you or your child need a measles vaccine: Measles Vaccine Recommendation Flowchart