
Welcome to the June 2024 ND Medicaid provider newsletter and thank you for caring for our members.
“Great opportunities to help others seldom come, but small ones surround us every day.” - Sally Koch
New services effective April 1, 2024

Preventive Medicine Counseling Risk Factor Reduction
These preventive services are for individuals without specific illnesses or conditions, but who are at risk of developing certain conditions and who might benefit from counseling, anticipatory guidance and risk-factor reductions.
The following types of counseling and risk factor reductions are covered:
- Prevention of cavities in children younger than five
- Healthy weight and weight gain in pregnancy
- Healthy diet and physical activity for cardiovascular disease prevention in adults with risk factors
- Sexually transmitted infections for adolescents and adults
- Tobacco use in adolescents and children
- BRCA-related cancer, risk assessment
- Perinatal depression
- Weight loss to prevent obesity and related morbidity and mortality in adults
- Falls prevention in community-dwelling older adults
- Skin cancer prevention – all ages
- Obesity in children and adolescents
- Breastfeeding
Preventive Medicine Counseling Risk Factor Reduction coverage requirements are located in the Preventive Services and Chronic Disease Management Policy.
Screening, Brief Intervention, and Referral to Treatment (SBIRT)
SBIRT is meant to prevent or reduce substance use through early intervention. This can prevent health-related consequences, diseases, accidents and injuries related to substance use.
SBIRT is an evidence-based, early intervention for people with substance use disorders and those at risk of developing those disorders.
SBIRT coverage requirements are located in the Preventive Services and Chronic Disease Management Policy.
Interprofessional Consultations
This service allows treating providers to consult with a specialist to assist the treating provider in diagnosis and/or management of a patient’s health condition without requiring the patient to have face-to-face contact with the specialist. Specialists bill for their consultation time with these codes.
Interprofessional Consultation requirements are located in the Telehealth Policy.
Prior authorization website redesign

The ND Medicaid prior authorization website has migrated to a new URL.
Save this link for the new landing page: ndmedicaid.acentra.com
The above link replaces the previously used www.hidesigns.com/ndmedicaid, which is now being redirected to the new landing page.
This website hosts ND Medicaid’s preferred drug list with coverage criteria, drug prior authorization forms, ND Medicaid Drug Use Review Board information and provider education material.
Updated direct links for other important pages are included below. You can also navigate to these pages through the drop-down menus at the top of the landing page.
- Preferred drug list: ndmedicaid.acentra.com/ndpdl
- Prior authorization forms: ndmedicaid.acentra.com/prior-authorization
Paxlovid and Lagevrio coverage

Medicaid plans must cover all COVID-19 treatments until the end of the third quarter of calendar year 2024.
On Nov. 1, 2023, the manufacturers of Lagevrio and Paxlovid began a transition from distribution by the U.S. government to distribution through the commercial channel.
Paxlovid: No prior authorization required
- Through Dec. 31, 2024, ND Medicaid members can obtain Paxlovid directly at the pharmacy at no cost without having to enroll in the patient assistance program.
- ND Medicaid members may also obtain Paxlovid at no cost through the patient assistance program. paxlovid.com/paxcess or call 1 (877) 219-7225 (1-877-C19-PACK).
Lagevrio: Prior authorization required
- Approved under emergency use authorization, Lagevrio should only be used in cases where Paxlovid is not an option and the use of Lagevrio is a medically urgent need. Prior authorization will be used to verify that FDA-approved Paxlovid cannot be utilized.
- ND Medicaid members cannot receive Lagevrio through the patient assistance program operated by the manufacturer. Merck has published program information at merckhelps.com/LAGEVRIO or 1 (800) 727-5400.
Preventing and controlling oral diseases with fluoride varnish

Dental caries remains the most common chronic preventable childhood disease in the United States. The use of fluoride varnish is an effective way to prevent and, in some cases, stop dental decay.
The chart below shows the 2023 total number of ND Medicaid Health Tracks well-child visits (Procedure codes S0302 or 9938x / 9939x), the total Health Tracks well-child visits combined with the application of fluoride varnish and the total number of missed opportunities/pay points.
Missed opportunities are where fluoride varnish could have been applied as part of a Health Tracks well-child visit, which also resulted in a missed pay point for providers and local public health units.
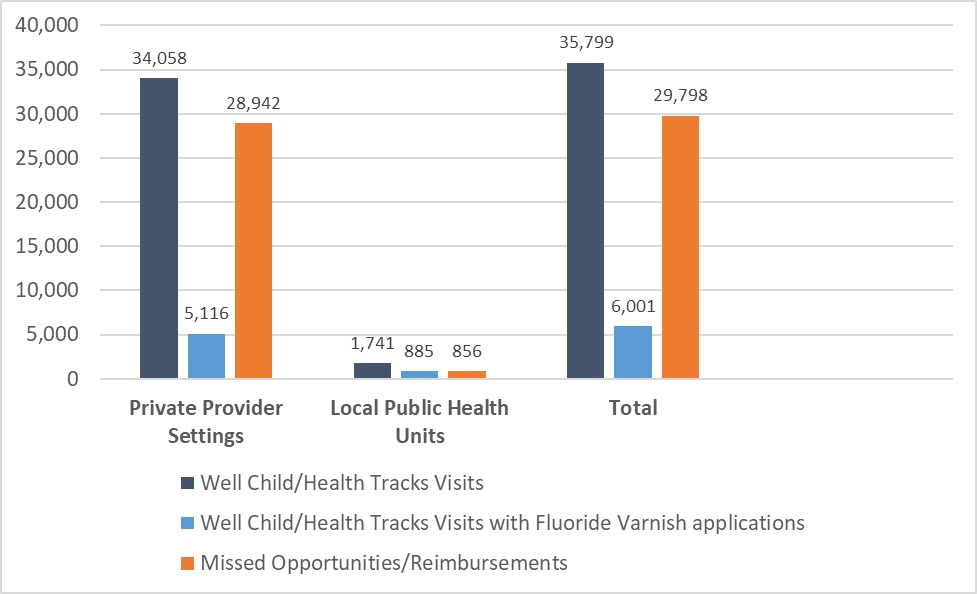
Almost 30,000 missed opportunities/pay points equals $853,200 in revenue between private provider settings and local public health units!
Fluoride varnish application is reimbursed at $28.44 as of Jan. 1, 2024.
How can providers help?
As a preventive measure, we are encouraging medical providers to integrate fluoride varnish applications into ND Medicaid Health Tracks well-child visits.
The Fluoride Varnish CPT© code for medical providers is 99188, which can be billed in addition to the Health Tracks well-child visit and/or other types of health care visits.
Fluoride varnish may be applied 2x/year for children without a service authorization. See Health Tracks Provider Outreach webpage for a toolkit with information on oral health, fluoride varnish and orthodontia.
If you would like to know the specific number of missed opportunities for your provider setting or you are interested in learning how your providers can begin to integrate fluoride varnish into your ND Medicaid Health Tracks well-child visits, reach out to us at htprovideroutreach@nd.gov.
To find a dentist who accepts ND Medicaid, visit InsureKidsNow.gov.
Learn more at hhs.nd.gov/health-tracks.
Providers, did you know you can help individuals apply for ND Medicaid?

You can do so in one of two ways: as an authorized representative or as a trusted partner.
Here's what you need to know.
Trusted Partners
Trusted partners work with trusted organizations or are professionals who provide education on programs and application assistance. They are considered a helper that assists many applicants and are limited to the information that can be exchanged. You should complete the application as a trusted partner if your relationship with the applicant is likely to end after the application process is complete.
Can a trusted partner sign the application on behalf of the applicant?
A trusted partner should never sign the application.
How do I become a trusted partner?
You will need to create an account in the self-service portal (SSP). There you will assist applicants in filling out applications, submitting documents and providing education on their case.
For help applying as a trusted partner, click here.
Authorized Representatives
This is a person who knows the applicant or family who will have the same responsibilities that the applicant/family would in the application process. Authorized representatives will be able to make informed decisions, receive notices, forms and updates.
You should complete the application as an authorized representative if you are someone who is close to the applicant and can help answer sensitive questions about their situation.
Can an authorized representative sign the application on behalf of the applicant?
This depends on the program they are applying for:
- The Supplemental Nutrition Assistance Program (SNAP), ND Medicaid and the Low Income Home Energy Assistance Program (LIHEAP) allow for an authorized representative to sign the application.
- An authorized representative should not sign an application for the Child Care Assistance Program (CCAP) or the Temporary Assistance for Needy Families (TANF).
How do I become an authorized representative?
You must be designated by the applicant, the applicant’s spouse or another responsible member of the household.
This can be done in writing or by completing the authorized portion on the application through the SSP or on the paper application.
For help applying as an authorized representative, click here.
Share our Medicaid Member E-News!

We are sending our Medicaid Member E-News to members every other month. E-News has updates on ND Medicaid programs, helpful reminders for staying healthy, how to get the most of members’ Medicaid coverage and other news they can use!
We’d love to partner with providers to spread the word about Medicaid Member E-News!
Please consider printing our flyer and displaying it in areas of your facility visited by ND Medicaid members.
Click on flyer to download.
Reminder: Ordering/Referring/Prescribing (ORP) Provider NPIs required on claims

Effective May 1, 2024, ND Medicaid requires the NPI of the ordering/referring/prescribing (ORP) be submitted on claims.
List of services requiring an ORP NPI
Academic Detailing meetings

Academic detailing: ndmedicaid.acentra.com/academic-detailing/#academic-detailing
Academic Detailing meetings will be hosted by Acentra Health via Microsoft Teams to provide information about ND Medicaid initiatives and desired outcomes, including updates to the preferred drug list and prior authorization forms.
Information will be provided by Russell Moore, Medicaid pharmacy specialist, Acentra Health.
If you wish to receive emails regarding quarterly Academic Detailing meetings:
- Email ndacademicdetailing@acentra.com with subject line “Join Email List”
- Include your practice site or pharmacy information
Acentra Health - Vendor for expanded provider reviews

Background: Acentra Health (formerly known as KEPRO) has been a vendor of the ND Medicaid program since 2021. Acentra processes certain service authorizations and completes retrospective reviews of inpatient and outpatient hospital claims.
What’s Changing: Acentra is expanding provider reviews with new focus areas including emergency room visits, behavioral health services, applied behavioral analysis and evaluation and management services for members in nursing facilities.
What to Expect: Your organization may be contacted by Acentra to request information about services you provided to ND Medicaid members. These requests are legitimate and are intended to inform more robust policies and guidance for providers.
Questions: contact Nicole Weigel at nmweigel@nd.gov. See https://nddhs.acentra.com/ for more information.
Preferred drug list changes

Insulin Updates
Novolog and insulin aspart require prior authorization.
Apidra (insulin glulisine) requires prior authorization.
Fiasp (insulin aspart) does not require prior authorization, but does require an electronic lookback for a 3-month supply of Humalog within the past 180 days in claim history.
Please begin transitioning members currently on Apidra, Novolog or insulin aspart to Humalog or insulin lispro to avoid disruption to insulin treatment.
GLP-1 Agonist Updates
- Ozempic, Rybelsus, and Bydureon Bcise are covered after a trial with Victoza with 2 other antihyperglycemic agents.
- Trulicity requires a trial of Ozempic with 2 other antihyperglycemic agents.
- Victoza is still covered without prior authorization.
Omnipod Updates
ND Medicaid no longer restricts Omnipod coverage by age.
Please consider if a tubeless pump is preferable for members receiving less than 66 units/day.
Asthma/COPD Product Updates
Symbicort requires prior authorization.
- Dulera (which contains formoterol) may be used for SMART (single inhaler for maintenance and rescue therapy) as recommended by the GINA (Global Initiative for Asthma) guidelines.
- The Dulera quantity limit allows up to 2 inhalers per 30 days (not to exceed a total of 9 inhalers per 182 days) for maintenance and rescue utilization.
Proton Pump Inhibitor Updates
Dexilant and Konvomep require prior authorization.
Otic Anti-Infectives
Ciprofloxacin/dexamethasone requires prior authorization.
ND Medicaid now covers Firesafe Cannula Valves
 Firesafe Cannula Valves make oxygen therapy safer. They help reduce the risk of fires by isolating the oxygen flow and putting out a fire that may travel back along the oxygen delivery tubing. These valves are meant to be installed in the oxygen delivery tubing or at the interface with the oxygen supply equipment.
Firesafe Cannula Valves make oxygen therapy safer. They help reduce the risk of fires by isolating the oxygen flow and putting out a fire that may travel back along the oxygen delivery tubing. These valves are meant to be installed in the oxygen delivery tubing or at the interface with the oxygen supply equipment.
It's recommended that each oxygen delivery circuit have two Firesafe devices. The first should be placed near the oxygen supply source, and the second near the patient.
Providers are required to submit claims for the Firesafe device using the Current Procedure Terminology (CPT) code E0700. Each valve is considered one unit, and the cost for each unit is $6.80. The limit is two units every six months.
If you have any inquiries, you can contact Tammy Holm, durable medical administrator at tamholm@nd.gov or (701) 328-2764.
Stay in the know! ND Medicaid provider newsletter subscription

Signing up to receive ND Medicaid’s quarterly provider newsletters is easy.
Step 1: Go to the Provider webpage.
Step 2: Enter your email address and click submit.
Step 3: Follow directions to set up and choose your subscription options. Select Medicaid Provider Newsletter.

